The Eye of The Storm
Author: Hamza Shah, OD, MS
A 74-year-old Asian woman, who had been receiving treatment for neurotrophic keratitis and severe dryness, recently presented with persistent sensations of a foreign body in her left eye, along with heightened light sensitivity and a decline in visual acuity. Her symptoms onset approximately 2-3 days ago.
Ophthalmic History:
- Meibomian gland dysfunction in both eyes (OU)
- Neurotrophic keratitis in both eyes (OU)
- Superficial punctate keratitis in both eyes (OU)
Medical History:
- Rheumatoid arthritis
- High cholesterol
- Gastroesophageal reflux disease (GERD)
- Hypertension
Entrance Exam Findings:
| OD | OS | |
|---|---|---|
| VAcc | 20/25 | 20/100 -1 [1mo ago 20/50] |
| Pupils | PERRL, (-)APD | PERRL, (-)APD |
| CVF | FTFC | FTFC |
| EOM | FROM | FROM |
Slit-Lamp and Posterior Findings:
| OD | OS | |
|---|---|---|
| Adnexa | Normal | Normal |
| L/L | 2+ telangiectasia w/ scalloped margins, 2+ MGD, puncta plug LL | 2+ telangiectasia w/ scalloped margins, 2+ MGD, puncta plug LL |
| Conj. | 1+ injection | 3+ injection, tr staining |
| Sclera | White/quiet | White/quiet |
| Cornea | 1-2+ diffuse SPK | 2-3+ diffuse SPK, 1+ filaments, 1mmHx2mmV superior peripheral opaque opacity w/ shallow overlying soft staining |
| Angle | 3-4+ | 3-4+ |
| A/C | Deep/quiet | tr cells |
| Iris | Normal | Normal |
| Lens | Clear | Clear |
| IOP | 17 | 17 |
| C/D | 0.30 | 0.20 |
| Optic Disc | (-)edema, (-)neo, (-)pallor | (-)edema, (-)neo, (-)pallor |
| Vitreous | Normal | Normal |
| Macula | Normal contour and reflex | Normal contour and reflex |
| Vessels | 2/3 ratio of arterioles/venules w/o tortuosity | 2/3 ratio of arterioles/venules w/o tortuosity |
| Posterior Seg | No holes/tears/breaks | No holes/tears/breaks |
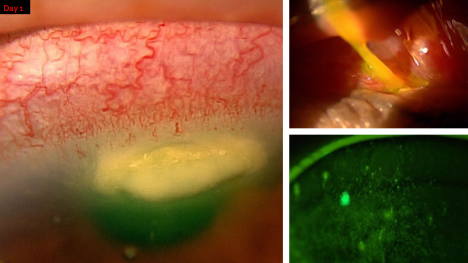
Figure 1: Superior corneal lesion, mucus at the punctual area, cornea SPK with filaments
Diagnosis:
Peripheral ulcerative keratitis
Figure 2: corneal appearance on day 1, day 29 (last slit-lamp photos), day 33 (telehealth visit)
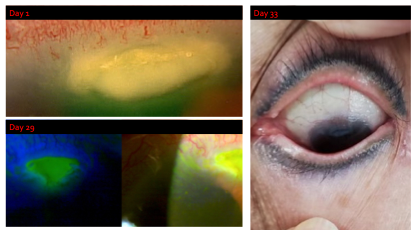
Figure 2: Timeline through which patient was managed.
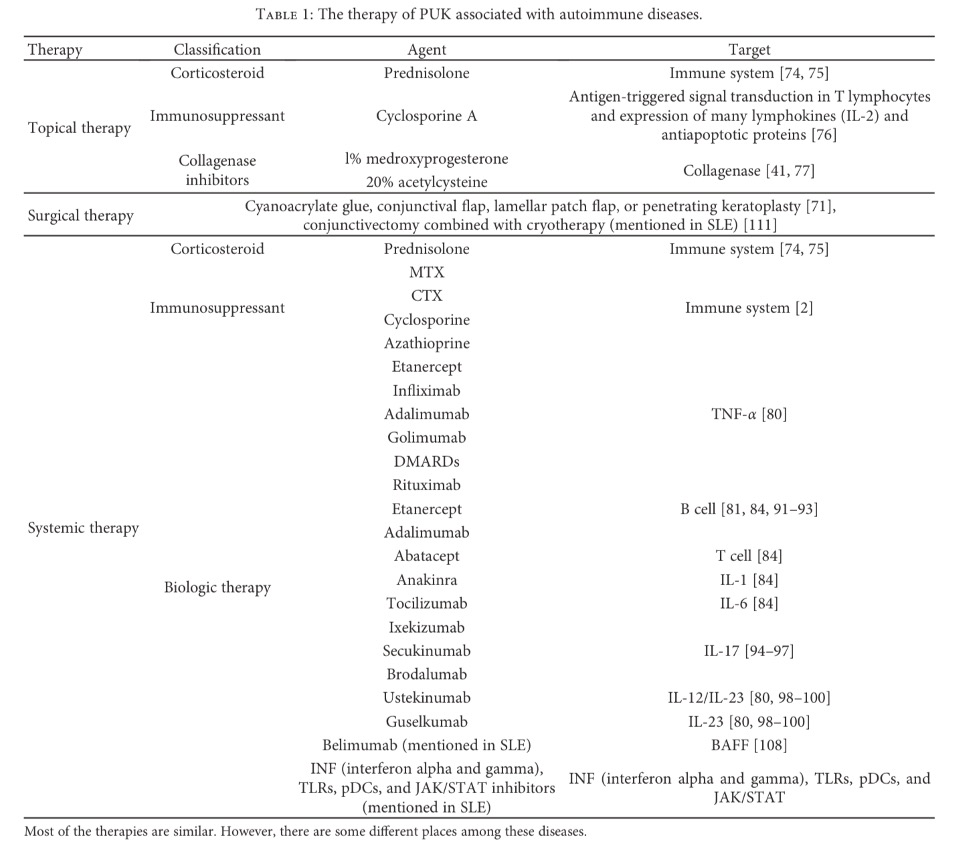
Figure 3 shows appropriate therapies that can be used for the Tx of PUK. Obtained from: DOI: 10.1155/2017/7298026.
Discussion:
When managing a lesion as such, it’s crucial to initially treat it as infectious and monitor the patient closely until culture results are available. If an infectious cause is ruled out and peripheral ulcerative keratitis (PUK) is suspected, appropriate treatment and testing can begin. PUK is often associated with systemic inflammatory conditions such as rheumatoid arthritis.
I recommend ordering blood tests (CBC, ESR, ACA, ANA, and Rh factor) regardless of whether the patient is diagnosed with a PUK-related condition (such as rheumatoid arthritis, polyarteritis nodosa, inflammatory bowel syndrome, or collagen vascular diseases like lupus) or not. Effective communication with a rheumatologist is essential to adjust systemic therapy as needed.
While systemic therapy is being adjusted, the patient may be treated with a combination of steroids (both drops and/or pills), amniotic membrane, doxycycline, vitamin C, and/or topical immunomodulators. Managing PUK often requires a comprehensive approach that integrates both oral and topical therapies. Given the inflammatory nature of PUK, treatment with topical and oral immunosuppressants is critical. For cases resistant to topical and oral steroid treatments, patient may need to be treated with immunosuppressives or biologics through rheumatology.
Repository corticotropin injection (acthar gel and purified cortrophin gel) are an emerging therapy for inflammatory ocular conditions such as PUK. This is an injection that has an anti-inflammatory and immunomodulatory mechanism. The MOA can be viewed on the package inset for Acthar gel.
[1] Cao Y, Zhang W, Wu J, Zhang H, Zhou H. Peripheral Ulcerative Keratitis Associated with Autoimmune Disease: Pathogenesis and Treatment. J Ophthalmol. 2017:7298026.