Not Just a Floater
Author: Hamza Shah, OD, MS
Case History
The patient presents for an annual diabetic eye examination. She mentioned that her visual acuity was fine until around a month ago when she noticed a significant floater in her left eye (OS). This floater appeared over a month ago and resembles a blood-like branch. There has been slight improvement in the floater's condition. She denied experiencing any flashes and emphasized the need to verify her insurance coverage before considering any laser intervention, as she cannot afford to pay out-of-pocket. Blood sugar levels are within the normal range. The patient is currently using an insulin pump, and her most recent A1C reading was ~>7.0%.
Ophthalmic History
- Proliferative diabetic retinopathy OU
- Pseudophakic OU
Medical History
- Type 2 Diabetes (>20 years)
- High cholesterol
- Hypertension
| Finding | OD | OS |
|---|---|---|
| Visual Acuity | 20/30 | 20/100 -1 |
| Pupils | PERRL, (-)APD | PERRL, (-)APD |
| CVF | FTFC | FTFC |
| EOM | FROM | FROM |
| Finding | OD | OS |
|---|---|---|
| Adnexa | Normal | Normal |
| L/L | 1+ dermatochalasis | 1+ dermatochalasis |
| Conj. | Clear | Clear |
| Sclera | White/quiet | White/quiet |
| Cornea | Clear | Clear |
| Angle | 3-4+ | 3-4+ |
| A/C | Deep/quiet | Deep/quiet |
| Iris | Normal | Normal |
| Lens | Clear | Clear |
| IOP | 17 | 17 |
| C/D | 0.40 | UTT |
| Optic Disc | (-)edema, (-)neo, (-)pallor | UTT |
| Vitreous | Normal | (-)schaffer sign, 3-4+ central vitreous hemorrhage |
| Macula | Few MA's | UTT |
| Vessels | Mild d/b hemes | UTT |
| Posterior Seg | 3+ PRP | 3+ PRP |
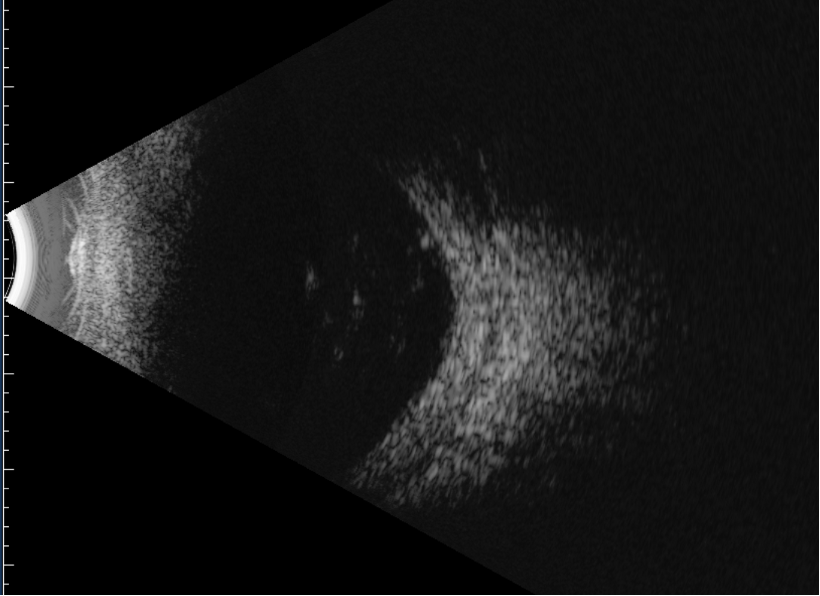
Figure 1: B-scan with a central vitreous hemorrhage, without retinal detachment.
Diagnosis
Vitreous hemorrhage due to advanced proliferative diabetic retinopathy
Discussion
When dealing with a patient with floaters, it is essential to consider a posterior vitreous detachment (PVD), which is the separation of the posterior vitreous cortex from the internal limiting membrane (ILM) of the retina. The vitreous adheres to the retina in the following order from strongest to weakest: vitreous base, optic nerve, macula, and blood vessels. Risk factors for developing a PVD include age, female gender, myopia, trauma, ocular surgery, inflammation, and underlying conditions such as retinitis pigmentosa (RP) or Stickler syndrome. The first signs to look for in a patient with a suspected PVD are the presence of Shafer's sign or a Weiss ring in the vitreous, which indicates that a PVD has likely occurred. However, there may still be attachments at the vitreous base, particularly in the peripheral retina, where most retinal holes or tears are diagnosed. It is important to remember that approximately 10% of symptomatic PVDs and 50-70% of PVDs accompanied by a vitreous hemorrhage will have an associated retinal hole or tear. PVD is commonly known as an age-related change.
The three most frequently encountered causes of vitreous hemorrhage (VH) include proliferative diabetic retinopathy (PDR), posterior vitreous detachment (PVD), and ocular trauma. Following a thorough examination to rule out the presence of any retinal hole, tear, break, or detachment, it is advisable to monitor the patient's condition over a period of 1 month. The patient should be seen every 1-2 weeks, with B-scan imaging, while the hemorrhage resolves.
In diabetic patients, ff there is no improvement within the specified timeframe (1 month), the patient may be considered for either anti-VEGF injections or pars plana vitrectomy as treatment options. Research studies have demonstrated that there is no statistically significant difference in visual acuity (VA) improvement between patients treated with Eyelea (administered as 3-4 injections spaced 4 weeks apart) and those who underwent vitrectomy with panretinal photocoagulation (PRP). Interestingly, it is worth noting that approximately one-third of the patients who initially received Eyelea treatment eventually required vitrectomy during the study.
[1] Antoszyk AN, Glassman AR, Beaulieu WT, et al. Effect of Intravitreous Aflibercept vs Vitrectomy With Panretinal Photocoagulation on Visual Acuity in Patients With Vitreous Hemorrhage From Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA. 2020;324(23):2383–2395. doi:10.1001/jama.2020.23027
[2] Ahmed F, Tripathy K. Posterior Vitreous Detachment. [Updated 2023 Aug 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563273/
[3] Bond-Taylor M, Jakobsson G, Zetterberg M. Posterior vitreous detachment - prevalence of and risk factors for retinal tears. Clin Ophthalmol. 2017;11:1689-1695.